New Insights into Normal Pressure Hydrocephalus
By: Noriana Jakopin and Dr. Jenna Koschnitzky, HA Director of Research Programs
Idiopathic Normal Pressure Hydrocephalus (iNPH) occurs when there is an abnormal accumulation of cerebrospinal fluid (CSF) which causes ventricular enlargement, often with a limited increase in intracranial pressure (ICP). The core clinical symptoms consist of cognitive impairment, gait disturbance, and urinary incontinence and are generally improved after treatment. However, it is estimated that less than one in five patients receive treatment, and there is limited information on the natural progression of iNPH.
A recently published study from researchers at the University of Gothenburg attempts to shed light on the long term outcomes of untreated iNPH by examining mortality rates, risk of dementia, and symptom progression in individuals with ventricular enlargement. The study was led by Daniel Jaraj, MD, PhD, a member of the HA Network for Discovery Science.
The research group obtained baseline information on the elderly population of Gothenburg, Sweden from 1986-2000. The study included 1,235 participants, all aged 75 or older. No patients with treated iNPH were included. Participants were divided into four groups based on radiological and clinical indications:
- Non-iNPH: consisting of participants who had no sign of ventricular enlargement upon computed tomography (CT) scan and did not exhibit any of the core clinical symptoms (cognitive impairment, gait disturbance, and urinary incontinence).
- Asymptomatic Hydrocephalic Ventricular enlargement (HVe): consisting of participants who showed ventricular enlargement but did not exhibit the core clinical symptoms.
- Possible iNPH: consisting of participants who showed ventricular enlargement and exhibited at least one of the three core clinical symptoms.
- Probable iNPH: consisting of participants who showed ventricular enlargement and exhibited gait disturbance as well as either cognitive impairment or urinary incontinence.
Five-year mortality rates were similar in non-iNPH patients, asymptomatic HVe patients, and possible iNPH patients. However, probable iNPH patients had a significantly higher five-year mortality rate of 87.5% (Table 1).

Table 1
Dementia developed in 20.6% of non-iNPH patients while 68% of patients who showed radiological indicators of iNPH (symptomatic HVe, possible iNPH, and probable iNPH) either had dementia at baseline or developed dementia during the study period.
Furthermore, almost all participants with enlarged ventricles showed some sign of symptom progression, and nearly 50% of asymptomatic HVe and possible iNPH patients developed probable iNPH during the time of the study period.

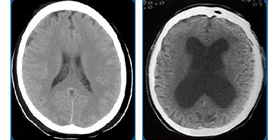
Figure 1
This study was unable to directly compare outcomes of untreated iNPH with treated iNPH. However, the authors hypothesize that radiological indicators (e.g. enlarged ventricles) develop before clinical symptoms (Figure 1). Surgical or other interventions at this early time-point may lead to better outcomes for iNPH patients.
For more information on this study click here.